Curriculum
We offer a variety of educational activities in order to reach everyone’s learning style. This includes morning report, bed side rounds, didactics, grand rounds, web-based modules, simulation training and home study opportunities.
Morning report is a crucial learning activity for residents. However, it is very important to have a robust and interactive morning report to avail this learning opportunity best. Our morning report format makes sure that night float gets to participate a couple of times per week in this important educational activity as well.
Morning report happens Monday-Friday from 8 a.m. to 8:30 a.m. This is a team led effort. The first part consists of arriving at the working diagnosis, using clinical reasoning and interactive questions from learners. The second part is a review of that working diagnosis where the teams can share quick learning points, a recent paper, or a podcast link to drive the learning points home.
Our Vice Chairman, Dr. Shawn Chillag is always present at morning report and has learning points for everyone. These sessions are a critical component of resident education in learning how different patient cases present, how to work them up and formulate treatment plans.
Goals of Morning report
- To relay important pieces from history and physical exam to derive an evidence based differential diagnosis (presenter).
- To ask hypothesis driven questions from history and physical to derive a robust differential (Audience).
- To accurately sum up and interpret labs/imaging. Focus on high value care.
- To come up with a formal diagnosis if available/possible.
- Spend 10 mins reviewing the case with focus on diagnosis and treatment and link to any interesting articles/findings/podcasts etc.
- Resident/Intern should be able to summarize the case in 2-3 minutes.
- Team effort.
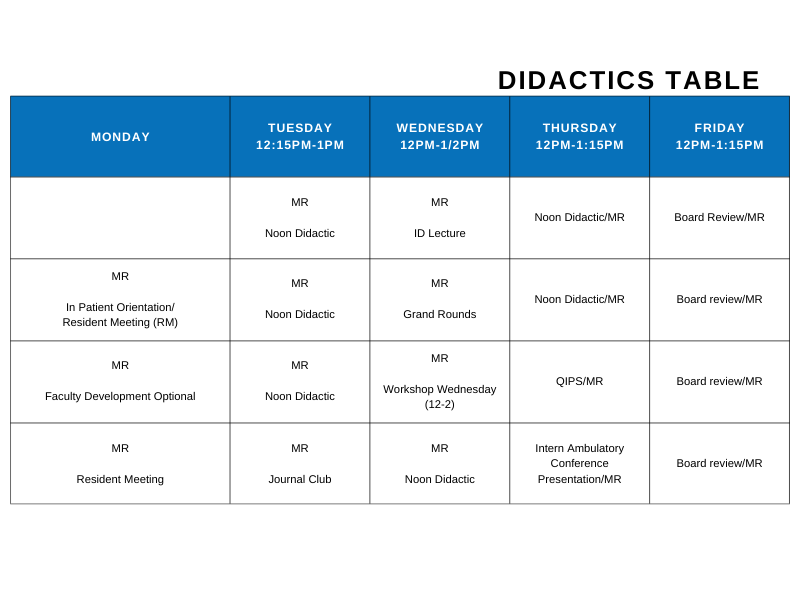
We select didactic curriculum based on the in-training exam topics and American Board of Internal Medicine certification blueprint. We strive to reinforce and highlight the most board relevant topics. Didactics are given Monday-Friday. Our didactics include a wide range of topics, not only covering the ABIM blueprints, but also: journal club, quality improvement patient safety, pharmacy lectures, as well as subspecialist lectures.
Our residency program has a robust Quality Improvement and Patient Safety program. The program involves a mix of didactics including introducing the key concepts of quality improvement and patient safety such as QI methodology, change management and Just culture etc.
The residents apply this learning to the ongoing QI projects and work step by step through the DMAIC methodology with support from a designated faculty member.
Our current QI projects are focused on providing efficient, high quality and evidence-based care to our patients as well as trying to address healthcare disparities. Some of the ongoing residents’ projects are as follows:
- Improving the accurate code status documentation in patients with stroke, CHF, and COPD.
- Increasing the number of patients with the AMD in the resident clinic.
- Increasing the compliance of CHF discharge bundle in the patients admitted to the resident service.
In addition to this, residents are given opportunities to participate in different hospital committees working on various QI projects on a system wide level.
Sample Block Schedule (will vary year to year according to complement)
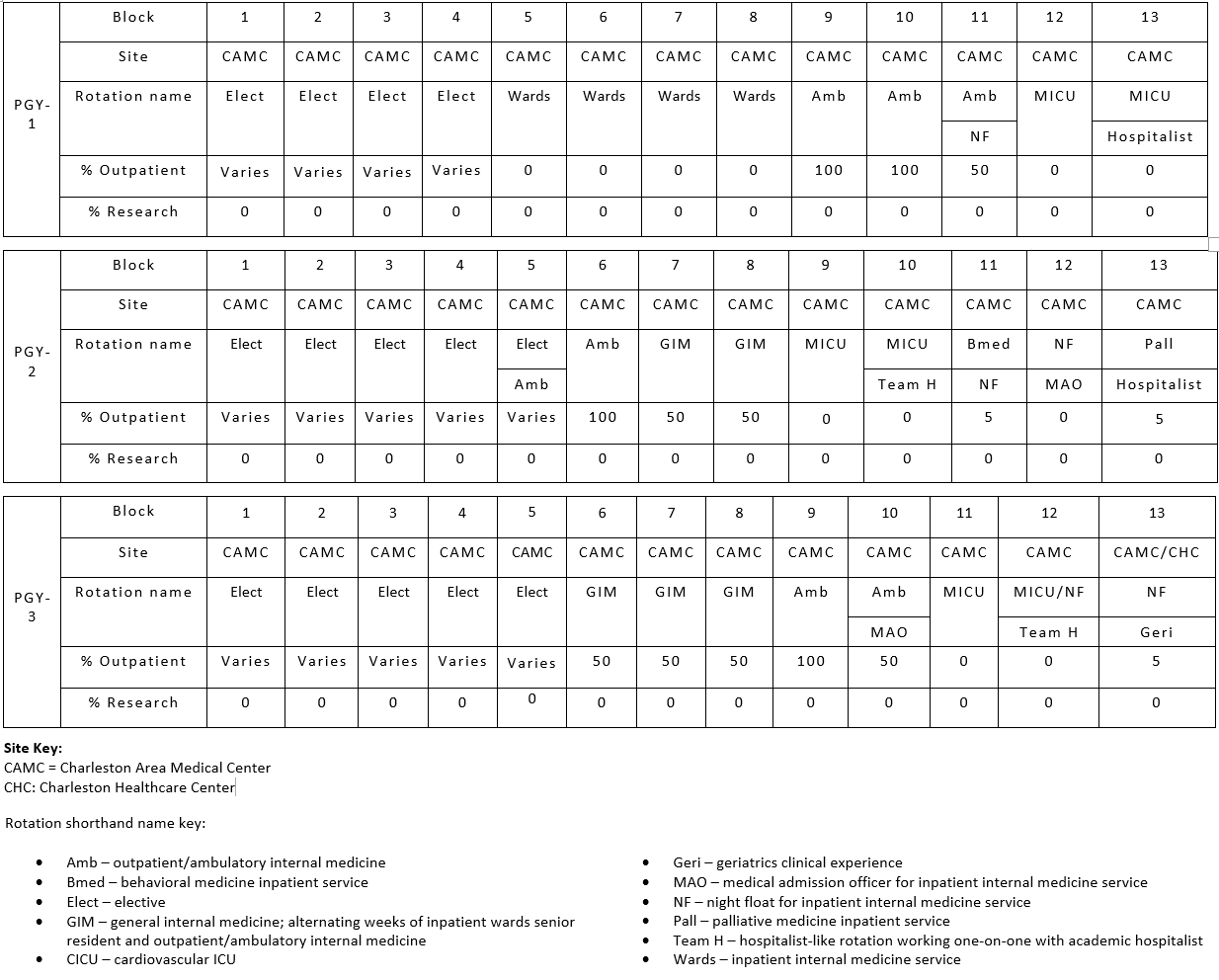
Rotation In Weeks | PGY1 | PGY2 | PGY3 |
Medicine Service | 16 | 12 | 10 |
Night Float | 4 | 6 | 4 |
ICU | 8 | 8 | 8 |
Ambulatory Clinic | 10 | 10 | 8 |
Electives | 14 | 12 | 22 |
4 weeks of Emergency Medicine Rotation as a senior resident.
Behavioral Medicine, Cardiology, Endocrine, Emergency Medicine, Gastroenterology, Geriatrics, Hematology-Oncology, Infectious Disease, Nephrology, Neurology, Palliative Care, Pulmonology, Rheumatology
- Allergy/Immunology
- Anesthesia
- Away rotation
- Cardiac ICU
- Clinician-educator track
- Dermatology
- Hospitalist
- Inpatient psychiatry
- Interventional radiology
- Obesity medicine
- Point-of-care ultrasound
- Research
- Women's health
We have monthly grand rounds with CME which focus on subspecialty topics as well as DEI related topics for interdisciplinary learning.
At our new simulation center, we will be holding monthly workshops to provide our residents hands on experience with POCUS and different procedures to provide robust experience for their learning.
The primary aim of the CET is to provide training that enables internal medicine residents with a career interest in medical education to develop the skills necessary to succeed as future clinician-educators.
The objectives for track participants are to:
- Advance the knowledge and skills for effective clinical teaching.
- Learn to design new curricula.
- Understand how to give feedback to learners and programs.
- Develop the skills needed to become a capable administrator, leader and change agent; and
- Master the skills necessary to investigate educational topics and disseminate scholarly work.
The primary aim of the Hospitalist Track is to provide additional clinical and educational training and mentorship to internal medicine residents who are interested in a Hospital Medicine career.
The objectives for track participants are to:
- Rotate through clinical experiences designed to help prepare residents for Hospital Medicine careers such as Point of Care Ultrasound (POCUS)
- Design and implement inpatient quality improvement projects
- Participate in a didactic curriculum focused on topics and metrics specific to Hospital Medicine
- Develop leadership and teamwork skills by participating in hospital committees
- Receive dedicated mentorship from experienced Hospitalists
Research and Simulation Learning
CAMC and the Department of Internal Medicine are committed to providing the necessary support for each of our learner's research needs. Whether your focus is in case presentation or original research, we have the tools in place to assist you through your project.
Suzanne Kemper, MPH, provides research support for the CAMC Department of Internal Medicine. Her role includes protocol development, IRB submissions/amendments, data collection design, analysis/results reporting, editing poster/presentations and manuscript development/submission.
Research focus areas include, but are not limited to, opioid use, liver cirrhosis, hepatitis A, gun ownership, heart failure and lung cancer screening. Abstract assistance for presentations/posters include CAMC Research Day (11 case/original posters/oral), WV State ACP (25 case/original posters, 2 orals) and National Conferences (19 case/original posters/oral presentations). Suzanne provides support on grant funded projects, including an American Cancer Society project related to lung cancer screening. She also guides and mentors Everest Institute candidates, as well as Summer Externs, during their time on campus. IM QIPs projects will become a vital part in how quality research can translate to practice. The reporting of IM Research is maintained via New Innovations.
Learn more about Research at CAMC
Simulation Center

The CAMC Center for Learning and Research maintains a full-time staff, including a curriculum development specialist who will assist faculty members with integrating simulation into their curricula. Simulation technology has advanced in recent years to allow for high-fidelity experiences that, when used as part of a larger educational experience, can greatly enhance medical education.
The Internal Medicine department utilizes the Center for Learning and Research for the following:
- Videoed Standardized patient for all interns
- Procedural Simulation
- Ultrasound assisted Central Lines
- Paracentesis
- Thoracentesis
- Lumbar Puncture
- Peripheral IV
- Venipuncture
- Pap exams
- Patient Simulation in following scenarios:
- Obtaining code status
- Breaking bad news
- Obtaining consent